Estrogen Dominance: Unpacking Hormonal Imbalance and its Manifestations
For many women experiencing perplexing symptoms, the question “Could this be hormonal?” is a frequent, yet often dismissed, concern. Historically, the conventional medical response to complex female hormonal issues, especially

For many women experiencing perplexing symptoms, the question “Could this be hormonal?” is a frequent, yet often dismissed, concern. Historically, the conventional medical response to complex female hormonal issues, especially those related to menstrual cycle irregularities or perimenopause, has often been limited.
Common advice might involve being told symptoms are “normal,” or the prescription of oral contraceptives—a choice that can suppress the natural rhythm of the hypothalamic-pituitary-ovarian (HPO) axis and, in some cases, decrease endogenous testosterone levels, potentially leading to side effects like a reduction in libido.
A more comprehensive, patient-centered approach requires diligent listening, sophisticated diagnostic thought, and individualized hormonal testing. This is particularly true as women enter perimenopause, a period defined by significant, often turbulent, hormonal transitions. Dismissing the profound somatic and psychological symptoms of perimenopause as merely a “normal part of aging” overlooks the genuine endocrine shifts that can dramatically impact a woman’s quality of life.
For many, these hormonal changes manifest as symptoms that can mimic or exacerbate mental health conditions, leading to misdiagnosis and the inappropriate prescribing of antidepressants rather than addressing the underlying hormonal imbalance.
A detailed investigation often reveals an identifiable physiological pattern, one of the most common being Estrogen Dominance.
Defining Estrogen Dominance
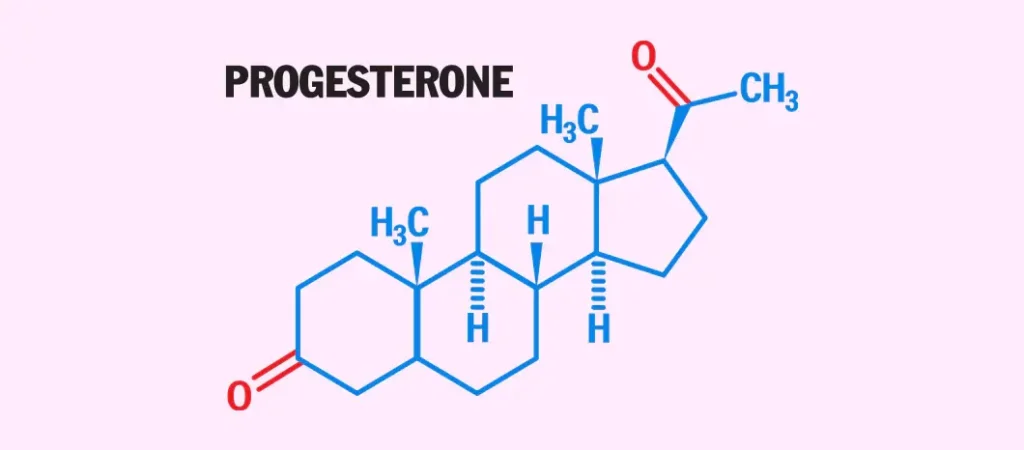
Estrogen Dominance is not necessarily defined by an absolute excess of estrogen, but rather by a supraphysiological ratio of estrogen relative to progesterone. This imbalance disrupts the delicate interplay between these two principal female sex hormones, which must be maintained for optimal health.
This state can arise from several distinct mechanisms:
● Elevated Estrogen Production: An increase in the synthesis of estrogen (e.g., from adipose tissue, or due to environmental exposures).
● Impaired Estrogen Metabolism/Elimination: A slowed rate of estrogen breakdown and excretion by the liver and gut, leading to the recirculation of active estrogen metabolites.
● Reduced Progesterone Production: This is a hallmark of perimenopause, where cycles can become anovulatory (lacking ovulation), which is the event necessary for the corpus luteum to produce adequate progesterone.
● Exposure to Xenoestrogens: External exposure to synthetic, endocrine-disrupting chemicals (EDCs) that mimic or potentiate the effects of endogenous estrogen in the body.
10 Common Clinical Manifestations of Estrogen Dominance
The clinical presentation of Estrogen Dominance is highly variable, reflecting the systemic actions of estrogen across multiple organ systems. The following are ten frequently observed signs:
- Menstrual Irregularities: Unpredictable cycle lengths, or changes in the timing or flow of menses.
- Menorrhagia (Heavy Periods): Excessive or prolonged menstrual bleeding, often resulting from unopposed estrogen stimulating excessive endometrial proliferation.
- Exacerbated Premenstrual Syndrome (PMS): Intensification of physical and emotional premenstrual symptoms.
- Gastrointestinal Distress/Bloating: Often related to fluid retention or altered gut motility.
- Breast Tenderness (Mastalgia): Pain or sensitivity in the breast tissue.
- Fibrocystic Breast Changes: The development of benign, lumpy, or dense breast tissue.
- Diminished Libido: A notable reduction in sexual desire.
- Cephalgia (Headaches): Often cyclical in nature, including menstrual migraines.
- Emotional Dysregulation: Significant and sometimes volatile mood swings.
- Anxiety and Heightened Nervousness: Symptoms often misattributed solely to psychological distress.
Associated Health Risks and Differential Diagnosis
Estrogen Dominance is not merely a collection of uncomfortable symptoms; it is also an endocrine environment associated with a higher incidence of specific reproductive and oncological conditions. These include Polycystic Ovarian Syndrome (PCOS), uterine fibroids (leiomyomas), endometriosis, and an elevated potential risk for estrogen-sensitive cancers, such as certain forms of breast and uterine cancer.
Conclusion and Next Steps
It is critical to underscore that this information does not constitute medical advice. Establishing a definitive diagnosis of Estrogen Dominance requires a qualified healthcare professional to order and interpret specific hormone testing (e.g., blood serum, saliva, or urinary metabolite analysis) within the context of a woman’s full medical history and symptom profile.
The objective of raising awareness regarding Estrogen Dominance is to empower women to become better advocates for their health. This common, yet frequently overlooked, endocrine pattern can dramatically diminish a woman’s quality of life, and its recognition is the first step toward appropriate and targeted therapeutic intervention.
Stay tuned for the subsequent articles in this series, which will delve deeper into the specific etiologies, the role of lifestyle modifications, and nutritional or supplemental support strategies pertinent to managing Estrogen Dominance.
Ravoke.com proudly supports women’s health, advocating for education, empowerment, and awareness around hormonal balance and wellness.
About Author
Dr. Bryan Treacy’s journey began with over three decades of dedicated service as an Ob/Gyn. His extensive experience in women’s health laid a solid foundation in medical science and patient care. Recognizing the limitations of traditional medicine, Dr. Treacy transitioned to holistic health consultancy, merging scientific knowledge with a broader understanding of wellness.








