The Cancer No One Talks About: Why Bladder Cancer Remains in the Shadows
Bladder cancer doesn’t have a ribbon everyone wears. It doesn’t have A-list celebrity telethons or heartwarming “survivor” segments on daytime TV. For most people, it’s just not on the radar
Bladder cancer doesn’t have a ribbon everyone wears. It doesn’t have A-list celebrity telethons or heartwarming “survivor” segments on daytime TV. For most people, it’s just not on the radar — until it crashes into their life without warning.
That’s what happened to my uncle. A bit of blood in the toilet bowl. Some fatigue. A feeling he couldn’t shake. By the time doctors took it seriously, it was stage 3 muscle-invasive bladder cancer. Six months later, we were saying goodbye.
What’s even more heartbreaking? This story is not rare.
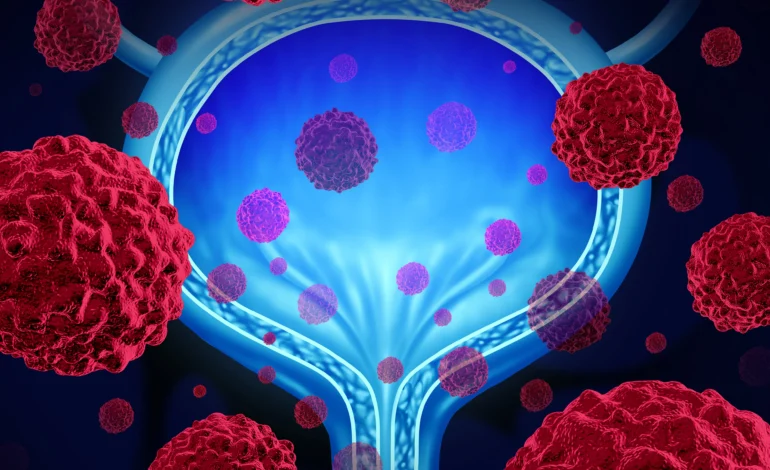
Bladder cancer affects over 82,000 Americans each year. It’s the fourth most common cancer in men, and yet it remains one of the least publicly discussed. The silence is deadly, and it needs to end.
Why Is Bladder Cancer So Under-Discussed?
One word: stigma.
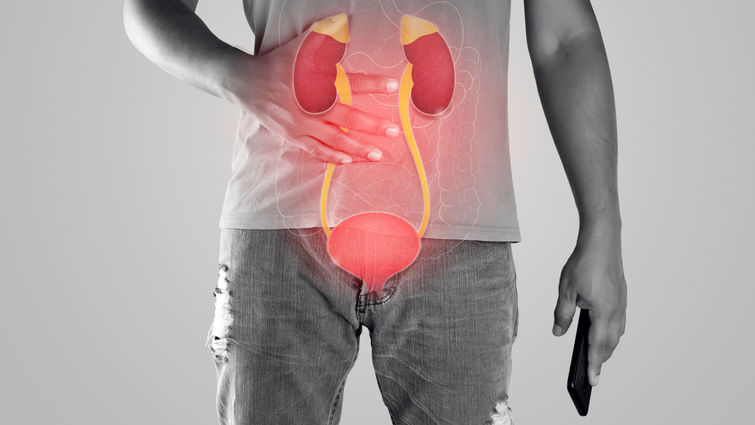
Bladder cancer is tied to parts of the body we don’t talk about in polite conversation. Urine, incontinence, urostomy bags, catheterization — these aren’t the things people bring up at dinner parties or support groups.
That shame keeps patients quiet, delays diagnosis, and isolates survivors.
Women often suffer most. Their symptoms — like urinary urgency or blood in the urine — are misdiagnosed as UTIs or menopause-related. As a result, women are diagnosed later and have worse outcomes than men.
Bladder Cancer: The Overlooked Killer
Bladder cancer affects over 82,000 Americans every year, according to the American Cancer Society. It’s the fourth most common cancer in men—and yet, it rarely makes headlines.
Men are four times more likely than women to get it, though women tend to be diagnosed later—and have poorer outcomes as a result.
Why? Because the symptoms are subtle. And often dismissed.
How It’s Diagnosed
If you or someone you love is experiencing bladder cancer symptoms, here’s what typically happens:
- Urine tests check for blood, infection, or cancer cells.
- Cystoscopy, where a thin tube with a camera is inserted into the bladder to look for tumors.
- Imaging scans (CT, MRI, or ultrasound) to check for spread.
- Biopsy to confirm cancer type and stage.
Early detection is everything. The 5-year survival rate for non-muscle-invasive bladder cancer is over 90%. But once it invades the muscle wall, survival rates drop significantly.
Celebrities Shining a Light on Bladder Health
Thankfully, some high-profile voices are helping to shift the narrative.
Deion Sanders
NFL legend Deion Sanders has openly shared his bladder and circulation issues, which resulted in multiple surgeries and even toe amputations. Though he hasn’t directly said “bladder cancer,” his journey has opened conversations around bladder health, kidney function, and systemic illness in men—especially Black men, who are disproportionately affected.
Sir Ian McKellen
The iconic actor known for Gandalf revealed he was undergoing regular scans and treatment after signs of early-stage bladder cancer. His decision to speak publicly has encouraged others to prioritize routine screening.
Read About: Blood Cancer Uncovered: What You Need to Know About the Silent Killer Affecting Millions
The First Signs You Should Never Ignore
Bladder cancer often whispers before it screams. By the time symptoms are severe, the cancer may already be advanced. Here’s what to look for right now:
Early Warning Signs:
- Blood in the urine (even once; pink, red, or cola-colored)
- Frequent urination, especially at night
- Painful or burning sensation when urinating
- Feeling like you need to go, but can’t
- Lower back or pelvic pain on one side
Men often think it’s just “getting older.” Women are told it’s a urinary tract infection. But both can be deadly assumptions.
If you experience any of these symptoms, ask for further testing. You have the right to be taken seriously.
Who You Should See: The Right Doctors Matter
Getting an accurate diagnosis and proper treatment can make all the difference. Bladder cancer is often misdiagnosed or mismanaged early on, so it’s crucial to see the right type of specialist.
Best Doctors to Consult for Bladder Cancer:
- Urologist
A bladder specialist who handles urinary tract conditions, including cystoscopies (scopes of the bladder) and TURBT (tumor removal). This is typically your first stop for diagnosis and treatment planning. - Urologic Oncologist
A urologist with advanced training in cancer. They are often the ones who perform bladder removal surgeries (cystectomies) and reconstructive procedures like neobladder creation. - Medical Oncologist
Handles chemotherapy, immunotherapy (like BCG), and systemic treatments. Essential for managing muscle-invasive or metastatic bladder cancer. - Radiation Oncologist
If you’re pursuing bladder-sparing treatment, you may undergo radiation with chemo. This doctor specializes in targeting tumors with minimal surrounding damage. - Pelvic Floor Therapist or Oncology Social Worker
Often forgotten, but hugely important for recovery, sexual health, and mental wellness after treatment.
Who’s at Risk? More People Than You Think
Several known risk factors increase the likelihood of developing bladder cancer:
- Smoking – Smokers are at least 3x more likely to get it.
- Chemical exposure – Especially from dyes, rubber, leather, or paint industries.
- Radiation or chemotherapy history (especially cyclophosphamide).
- Chronic bladder infections or inflammation.
- Age – Most are diagnosed over 55.
- Gender – Men are more likely to get it, but women die from it more often due to delayed diagnosis.
What’s Being Done For Bladder Cancer Treatment?
Bladder cancer has lagged behind in research funding for decades—but that’s finally beginning to change. More organizations and institutions are investing in better detection tools, new bladder cancer treatments, and, ultimately, a cure.
Current Research Highlights:
- Immunotherapy Advancements: Drugs like Atezolizumab and Nivolumab are helping the immune system target bladder cancer cells, especially for advanced stages.
- Targeted Therapy: Precision medicine is being used to analyze the tumor’s DNA and customize drugs that attack specific mutations.
- Non-Invasive Detection Tools: Urine-based genetic tests like Cxbladder and UroSEEK aim to detect bladder cancer early, reducing the need for invasive procedures.
- Bladder Preservation Studies: Ongoing clinical trials are exploring how to safely avoid radical cystectomy (bladder removal) by combining chemo, radiation, and immunotherapy.
- Artificial Intelligence in Cystoscopy: New tools are being developed to help doctors identify tumors earlier and with greater accuracy during bladder scopes.
While a definitive “cure” hasn’t yet emerged, progress is real—and it’s accelerating.
Treatment Options: Personalized and Evolving
For Early-Stage (Non-Muscle-Invasive):
- TURBT surgery – Removal of the tumor via scope.
- BCG therapy – An immunotherapy injected directly into the bladder.
- Intravesical chemo – Targeted, bladder-only chemotherapy.
For Advanced (Muscle-Invasive or Metastatic):
- Radical cystectomy – Full bladder removal, often with reconstruction (urostomy or neobladder).
- Systemic chemotherapy
- Checkpoint inhibitors – Immunotherapy drugs targeting cancer cell defense mechanisms.
- Radiation therapy
Every case is different. A multidisciplinary team is often the best way forward.
The Emotional Reality No One Warns You About
Even after successful treatment, bladder cancer changes lives forever.
Many survivors struggle with:
- Incontinence
- Sexual dysfunction
- Body image issues
- Depression or anxiety
- Relationship difficulties
There are very few support networks compared to other cancers. Survivors often report feeling invisible—even within cancer communities.
We Need to Talk Louder
The silence around bladder cancer isn’t just frustrating – it’s fatal.
Too many lives are lost simply because people were too embarrassed to ask for help. Or because doctors dismissed bladder cancer symptoms. Or because there wasn’t enough research funding to find better tools.
Let’s change that.
Talk about your bladder. Share this article. Normalize checkups. And if you’re living with this disease, know this: you are not alone, and you deserve to be heard.
FAQs
1: What is the most common early warning sign of bladder cancer?
A: The most common and often the first sign of bladder cancer is hematuria, or blood in the urine. It might be visible (making urine look pink, red, or cola-colored) or only detectable under a microscope. Even a single occurrence should never be ignored, as early detection is critical for a high survival rate.
2: I have symptoms; what type of doctor should I see for bladder cancer?
A: Your first step should be to see a Urologist. They are specialists in the urinary tract and will perform initial tests, such as a urine test or cystoscopy. If cancer is found, you will likely also consult a Urologic Oncologist (a surgeon specializing in urologic cancers) and potentially a Medical Oncologist for systemic treatments like chemotherapy or immunotherapy.
3: Why is bladder cancer considered an “overlooked” or “silent” cancer?
A: Bladder cancer remains in the shadows primarily due to stigma, as it involves bodily functions and parts (like urine and catheters) that people are often uncomfortable discussing. This silence leads to delayed diagnosis, especially in women whose symptoms are frequently misdiagnosed as UTIs. Furthermore, it receives significantly less public awareness and research funding compared to other common cancers.