Measles Cases Rising in 34 States: How It Affects Your Body, Who’s at Risk, and How to Stay Safe
Measles cases are surging in 34 states. Learn how the virus affects your body, why it’s serious, which communities are most impacted, and how vaccination protects you.
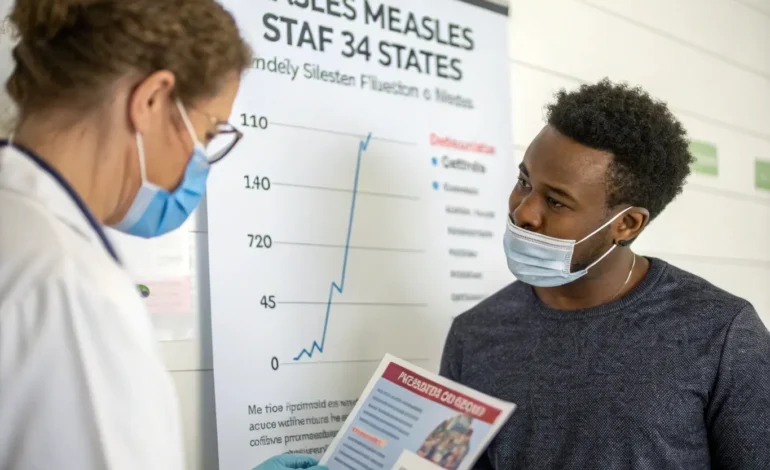
After decades of being nearly eradicated in the United States, measles is making a disturbing comeback. As of June 2025, health officials have confirmed measles cases in 34 states, marking the most extensive outbreak since the early 1990s. This resurgence raises urgent questions: Why is measles spreading again? How serious is the illness? Who is most vulnerable? And what steps can you take to protect yourself and your loved ones?
This article dives deep into these questions, exploring the science behind measles, its impact on the body, the communities most affected, and practical prevention measures.
Understanding Measles: More Than Just a Rash
Measles is caused by the measles virus, a highly contagious pathogen that attacks the respiratory system before spreading throughout the body. It primarily transmits through airborne droplets released when an infected person coughs or sneezes, lingering in the air for up to two hours. This means that even brief exposure in shared spaces, like waiting rooms or public transport, can lead to infection.
The initial symptoms often resemble a cold or flu:
- High fever (which can exceed 104°F)
- Persistent cough
- Runny nose
- Red, watery eyes (conjunctivitis)
About 3 to 5 days after symptoms start, the classic measles rash appears. It begins as flat red spots at the hairline and spreads downward to cover the face, neck, torso, arms, legs, and feet. The rash can last 5–6 days and often coincides with the highest contagious period.
How Does Measles Affect the Body?
While the rash is a hallmark, measles is much more than a skin condition. The virus can cause profound and sometimes life-threatening complications by:
- Weakening the immune system: Measles infection suppresses the immune system for weeks or months, increasing vulnerability to other infections like pneumonia or ear infections. This immune suppression can wipe out immune memory, leaving survivors susceptible to illnesses they were previously protected against.
- Causing pneumonia: This is the leading cause of measles-related deaths worldwide, responsible for roughly 60% of fatal cases.
- Triggering encephalitis: Brain inflammation occurs in about 1 in 1,000 cases and can cause seizures, permanent brain damage, or death.
- Inducing blindness: Especially in malnourished children with vitamin A deficiency.
- Leading to miscarriage or premature birth in pregnant women infected with measles.
Measles-related deaths globally still number in the hundreds of thousands annually, predominantly in countries without widespread vaccination. While fatalities are rarer in developed countries, the risk remains real, particularly for infants, elderly adults, and immunocompromised individuals.
Measles vs. Chickenpox: What’s the Difference?
It’s common to confuse measles with chickenpox since both cause rashes and fever in children. However, they are distinct illnesses caused by different viruses with different patterns and severity:
| Feature | Measles | Chickenpox |
| Cause | Measles virus | Varicella-zoster virus |
| Rash Appearance | Flat or slightly raised red spots, starting on face and spreading downwards | Itchy, fluid-filled blisters all over body |
| Contagiousness | Extremely high — up to 90% transmission among unvaccinated contacts | Highly contagious, but less than measles |
| Vaccine Availability | MMR vaccine | Varicella vaccine |
| Severity | Can cause serious complications, including death | Usually milder, but can be severe in adults or immunocompromised |
Unlike chickenpox, there is no specific antiviral treatment for measles, and prevention through vaccination is the best defense.
Why Are Measles Cases Rising Again?
The resurgence of measles in 2025 is primarily due to declining vaccination rates in certain communities. The MMR vaccine (measles, mumps, rubella) has been highly effective at preventing outbreaks since its introduction in the 1960s, but coverage has dropped below the critical threshold of 95% needed for herd immunity in many areas.
Factors contributing to this decline include:
- Vaccine hesitancy fueled by misinformation and mistrust in medical institutions.
- Limited access to healthcare services in rural and underserved urban areas.
- Religious or philosophical objections to vaccination in some communities.
- International travel to and from countries experiencing active measles epidemics.
“Measles is incredibly contagious. Even small drops in vaccination coverage can trigger outbreaks,” explains Dr. Lena Harrell, infectious disease specialist at Johns Hopkins University. “Once the virus enters a community where many people are unvaccinated, it spreads rapidly.”
Who Is Most at Risk?
While anyone unvaccinated can contract measles, the following groups are particularly vulnerable to severe illness:
- Infants under 12 months, too young to be vaccinated.
- Pregnant women, as measles can cause miscarriage or premature birth.
- Immunocompromised individuals, including cancer patients, transplant recipients, and people with HIV/AIDS.
- Adults born between 1963 and 1967, who may have received an early version of the vaccine that was less effective.
The Disproportionate Impact on Communities of Color and Underserved Populations
Measles outbreaks don’t affect all populations equally. Data reveal that Black, Hispanic, Native American, and immigrant communities often face higher risks and worse outcomes due to:
- Healthcare disparities: Barriers like lack of insurance, transportation difficulties, and fewer nearby clinics reduce vaccine access.
- Crowded living conditions: Overcrowding increases transmission risk.
- Cultural and language barriers: These can impede vaccine education and outreach.
- Historical mistrust of healthcare systems stemming from past abuses.
“To effectively combat measles, public health responses must be culturally competent and address social determinants of health,” says Dr. Harrell.
What Can You Do to Protect Yourself and Your Family?
Vaccination remains the single most effective protection against measles. Here are critical steps to take:
- Verify your vaccination status: Adults unsure about their MMR vaccine history can get a blood test (titer) to check immunity.
- Ensure children get vaccinated on schedule: The CDC recommends two doses — the first between 12-15 months old and a second at 4-6 years.
- Practice good hygiene and isolate if sick: Measles is airborne; isolation and masking help prevent spread.
- Avoid travel to outbreak areas if you or your family are unvaccinated or at high risk.
- Educate and advocate: Help combat misinformation by sharing facts from trusted sources like the CDC and WHO.
Recognizing Symptoms and When to Seek Medical Help
Measles symptoms usually appear 7-14 days after exposure. If you experience high fever, cough, runny nose, red eyes, followed by a spreading rash, contact a healthcare provider immediately. Do not visit clinics or emergency rooms without calling first to prevent spreading the virus.
Early supportive care — including hydration, fever management, and vitamin A supplementation — can reduce complications.
A Call for Community Action
This outbreak is a stark reminder that diseases once controlled through vaccination can return if vigilance lapses. Combating measles requires coordinated efforts between healthcare providers, public health officials, community leaders, and individuals.
“Vaccination is not just a personal choice — it’s a community responsibility,” emphasizes Dr. Harrell. “Protecting those who cannot be vaccinated — infants, immunocompromised, and elderly — depends on everyone doing their part.”
New Perspectives
The return of measles challenges us to reconsider how we value scientific progress and public health infrastructure. It forces us to confront inequalities that have left many communities vulnerable.
Education, access, and empathy are our best tools to stop this outbreak and prevent future ones.






