HPV in Full: Decoding the Invisible Virus
Written by Matt Canada Brown for Ravoke.com Written on behalf of Ravoke.com for public dialogue, information, and relevant community stories. The included information in this story is not to be

Written by Matt Canada Brown for Ravoke.com
Written on behalf of Ravoke.com for public dialogue, information, and relevant community stories. The included information in this story is not to be taken as direct public health guidance, as each person’s circumstances differ. This article is written for informal relevance and awareness only.
For a virus that affects nearly every sexually active person at some point in their lives, Human Papillomavirus (HPV) remains shrouded in myth. It is the most common sexually transmitted infection (STI) globally, yet because it often leaves no trace, it is frequently misunderstood.
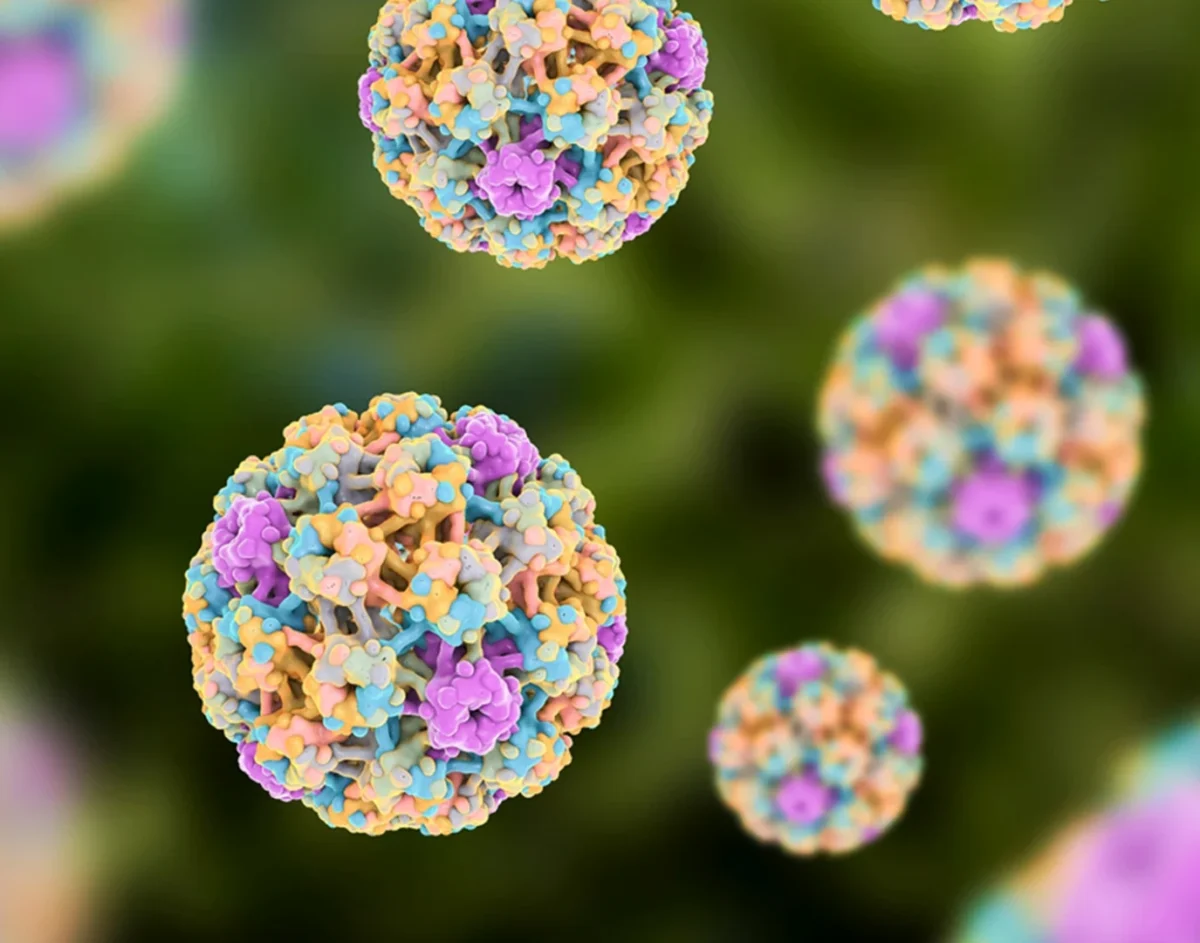
How HPV Works: The Stealth Invader
HPV is not a single virus, but a group of more than 200 related viruses. About 40 of these are considered “genital” types and are spread through direct skin-to-skin contact. Unlike many viruses that circulate through the bloodstream, HPV targets the basal epithelial cells—the deeper layers of the skin or mucous membranes in areas such as the cervix, throat, or anus.
Once the virus enters these cells, it typically follows one of two paths:
Low-Risk Strains
Examples: HPV 6 and 11
These strains typically cause benign growths such as genital warts. While uncomfortable or distressing, they do not lead to cancer.
High-Risk Strains
Examples: HPV 16 and 18
These strains can integrate their DNA into the host cell’s genome. Over years or even decades, this disruption can cause abnormal cell growth, leading to precancerous lesions and, eventually, cancer.
The Vaccine: A Prevention, Not a Cure
The HPV vaccine represents a major success in modern immunology. It uses Virus-Like Particles (VLPs)—empty protein shells that resemble the virus but contain no genetic material. These particles train the immune system to produce antibodies without causing infection.
If the body later encounters the real virus, these antibodies bind to it and prevent it from entering cells. The most widely used vaccine, Gardasil 9, protects against nine HPV strains responsible for approximately 90% of cervical cancers and 90% of genital warts.
A Global Shift: One Dose Protection
In a major adaptation, the World Health Organization (WHO) now recommends a single-dose schedule for individuals aged 9–20. Evidence shows that one dose provides comparable protection to the traditional two-dose schedule. This shift is considered a game-changer for global vaccine access, particularly in lower-income regions.
The Silent Nature of HPV
The vast majority of HPV infections—around 90%—are cleared naturally by the immune system within two years. Because the virus is often sub-clinical, producing no symptoms during this time, most people never realize they were carriers.
Testing options are also limited. While women may receive HPV co-testing during Pap smears, there is currently no approved, routine test for HPV in men or for HPV infections in the throat. This silent nature is why vaccination and routine screening remain the most reliable defenses.
Dormancy and Reactivation
There is also a critical dormancy factor. One of the most distressing scenarios for couples is a positive HPV result years into a monogamous relationship. HPV behaves like a slow-burning ember—it can remain dormant in the body for decades.
A positive test today may reflect exposure from 15 or even 20 years ago. As the immune system ages or experiences stress, particularly in cases of chronic illness or immune compromise, a dormant infection can reactivate and become detectable.
Our T-cells play a central role in keeping HPV suppressed. When the body is under systemic stress, that immune surveillance can weaken. For this reason, a new diagnosis is almost never a reliable indicator of recent infidelity. In long-term partnerships, HPV is often a shared “legacy” infection from the past.
Michael Douglas: From Stigma to Advocacy
In 2010, actor Michael Douglas was diagnosed with Stage IV throat cancer. Early reports focused on his history of smoking and alcohol use, but Douglas later publicly linked his cancer to HPV.
“Without wanting to get too specific, this particular cancer is caused by HPV… it’s a sexually transmitted disease that causes cancer.”
— Michael Douglas, 2013
His openness helped shift the global conversation around HPV. Douglas underwent aggressive chemotherapy and radiation, losing 45 pounds and enduring significant physical toll. Today, he remains cancer-free and is a vocal advocate for the Oral Cancer Foundation.
His story underscores a vital truth: HPV-related cancers are not just a women’s issue—they are a human health issue.
Men, HPV, and the Screening Gap
While cervical cancer has historically been the focus, the fastest-rising HPV-related cancer is oropharyngeal (throat) cancer, which disproportionately affects men.
Men are often excluded from screening discussions because there is no equivalent to a Pap smear for them. This gap makes vaccination for boys especially critical—not only to reduce cancer risk, but to dismantle stigma and misinformation.
Global Goals and Health Equity
Global health leaders, led by the WHO, have set an ambitious “90–70–90” target for eliminating cervical cancer by 2030:
- 90% of girls fully vaccinated by age 15
- 70% of women screened with a high-performance test by ages 35 and 45
- 90% of women with pre-cancer or cancer receiving treatment
By adopting single-dose vaccination strategies and promoting gender-neutral vaccination, public health systems are closing gaps in prevention.
This approach is especially critical in addressing the “Cervical Cancer Divide,” as nearly 90% of cervical cancer deaths occur in low- and middle-income countries. Single-dose strategies are not just medical solutions—they are tools for social justice and health equity.
Many global health forums, including those in Canada and the UK, are also moving toward HPV self-testing kits. These offer a major benefit for individuals with mobility disabilities or for those who find traditional pelvic exams traumatic or physically difficult.
Supporting Immune Dormancy
While there is no cure for HPV, certain lifestyle factors may help the immune system keep the virus dormant. Research suggests that folate and vitamin B12 play a role in cervical health.
Conversely, smoking is one of the highest risk factors for HPV-related cancer. Smoking weakens immune responses in the skin and mucosal tissues, allowing the virus to cause greater cellular damage over time.
Frequently Asked Questions (FAQ)
1. If I test positive after years of monogamy, does it mean my partner cheated?
No. HPV can remain dormant for decades. A positive result usually reflects an older infection that has recently reactivated.
2. Is there a test for men?
Currently, there is no routine, approved swab or blood test for men without symptoms. Vaccination remains the primary defense.
3. Can the vaccine help if I already have HPV?
The vaccine will not clear an existing infection, but it can protect against other high-risk strains you have not yet encountered.
4. Why is smoking so dangerous with HPV?
Smoking reduces the ability of immune cells in mucosal linings to suppress the virus, increasing the risk of cancerous changes.
5. Is the one-dose vaccine really enough?
Yes. Data adopted by the WHO shows that one dose produces a strong immune response in younger populations, comparable to multi-dose schedules.